Another interesting read.. those us who are not in the bar with the fatalists will end up knowing a bit about virology...

From here :
Thread by @angie_rasmussen: People are still freaking out over "asymptomatic" patients, so here's some info on virus incubation, symptoms, and lab confirmation of #nCoV…
People are still freaking out over "asymptomatic" patients, so here's some info on virus incubation, symptoms, and lab confirmation of
#nCoV2019 #coronavirus tests. It's not unusual for patients to test negative (for this or any other virus) in the early days after infection.
When a virus infects a cell, it takes time to replicate itself inside that cell and produce new virus particles. The period of time when a virus is replicating but hasn't yet begun producing new virus particles (called virions) is called the eclipse.
During the eclipse phase, viral RNA (the genetic material of the virus) and proteins are produced in cells. Proteins are involved in replicating the virus, hijacking host cell functions, evading immunity, and making the virus "shell" (capsid/structural proteins).
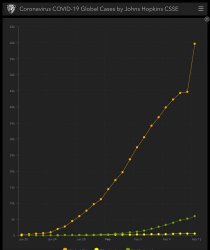
Viral RNA is packaged into the capsids and the virus particles are released from the cell. They go on to infect other cells nearby and the process repeats, resulting in exponential increases in the amount of virus (called titer)
Current virus testing technology (qRT-PCR) detects viral RNA. These tests are sensitive, but there's a limit of detection. qRT-PCR can only detect virus if there are sufficient viral titers. Early in infection, there may not be enough RNA to reliably detect this.
Also, cells in the human respiratory tract are highly structured. There are different kinds of cells that are organized into tissues. Not all of these cells are susceptible to infection, and certain cell types may produce more virus than others.
There are also natural barriers, such as mucus, that trap viruses and prevent them from infecting cells. So it can take time to achieve detectable virus titers. That time depends on a whole lot of variables.
Infectious dose, mode of transmission, viral genetics, viral fitness, host genetics, host cell receptor expression, antiviral response, amount of mucus, other underlying conditions, sampling procedure--these can all impact titer and hence the time it takes to detect infection
Note I haven't even mentioned symptoms. That's because symptoms are largely due to the host response to infection, rather than the infection itself (S/O to host responses, that's what I study!).
For coronaviruses, symptoms are generally the result of host cells (either infected cells or other immune cells nearby) detecting that infection and triggering antiviral responses. This process is complicated and plays out differently in every infected host.
It's kind of like a football game. There are different specialized players on each side and different coaching strategies. Sometimes the host keeps the virus in check, sometimes the other way around.
But when a virus is able to spread--for example, to the lower respiratory tract--then the host response also is more widespread. That response to viruses includes inflammation. Localized, controlled inflammation is good--it's needed for immune function to clear virus
More widespread, uncontrolled inflammation is bad. That's how a patient gets pneumonia. When this happens, a patient is definitely symptomatic. These patients have plenty of detectable virus.
However, a patient who is asymptomatic but still infected might not. If a patient controls the infection locally, they might not be shedding tons of detectable virus. They might still be capable of transmitting virus, albeit less capable than a patient who is very sick.
Similarly, a patient in the very early stages of infection may test negative because virus titers have not yet met the threshold for detection, regardless of the eventual severity of disease. In both situations, it is not unexpected to have a negative nasal swab test.
The important things to note are that "OMG this patient is asymptomatic" or "OMG this patient tested negative and later tested positive" are not abnormal. These are fully consistent with how viruses replicate, spread, and cause disease.
Asymptomatic patients generally don't transmit virus as efficiently, because they have lower virus titers and because they aren't experiencing clinical features that encourage virus spread (coughing, sneezing, excess mucus production).
And patients with negative test results early in infection may likewise be capable of spreading virus, but are also less likely to do so because they aren't shedding very much virus. This is expected. It's just viruses doing what viruses do.
So I wish the media and some scientists would cut out all the Typhoid Mary hysteria.
#nCoV2019 #coronavirus spread is not some aberration or a silent epidemic in which we'll all only find out we're doomed once it's too late.
We need to focus on improving testing, treating patients, and our fundamental understanding of virus pathogenesis (again, s/o to the host response!). The misdirected focus is harming our ability to adequately contain spread and is responsible for some truly coughty policy choices
The cruise ship sitch, involuntary quarantines and travel bans, confusing diagnostic criteria, criminalized epidemiology...these are all further complicating an already complex situation by fixating on this asymptomatic transmission issue, which, again, is just viruses virusing.